April 2021
Avoiding Athlete's Foot in the Locker Room
 Athlete’s foot is an infection of the skin on the feet that is caused by a fungus. Fungi thrive in warm, moist environments, such as locker room floors, and the fungus that causes athlete’s foot is highly contagious. Does this mean that you should avoid the gym? Not necessarily. Even if you frequent the locker room, there are steps that you can take to prevent a fungal infection. These prevention techniques include wearing flip-flops or other shoes while walking in the locker room, standing on a clean towel while changing to avoid direct contact between your feet and the floor, and washing and drying your feet thoroughly after exercising. If you or someone you know has developed athlete’s foot, it is suggested that you call and schedule an appointment with a podiatrist who can help treat this condition and teach you additional preventive measures.
Athlete’s foot is an infection of the skin on the feet that is caused by a fungus. Fungi thrive in warm, moist environments, such as locker room floors, and the fungus that causes athlete’s foot is highly contagious. Does this mean that you should avoid the gym? Not necessarily. Even if you frequent the locker room, there are steps that you can take to prevent a fungal infection. These prevention techniques include wearing flip-flops or other shoes while walking in the locker room, standing on a clean towel while changing to avoid direct contact between your feet and the floor, and washing and drying your feet thoroughly after exercising. If you or someone you know has developed athlete’s foot, it is suggested that you call and schedule an appointment with a podiatrist who can help treat this condition and teach you additional preventive measures.
Athlete’s foot is an inconvenient condition that can be easily reduced with the proper treatment. If you have any concerns about your feet and ankles, contact one of our podiatrists from Grobowski Foot & Ankle. our doctors will treat your foot and ankle needs.
Athlete’s Foot: The Sole Story
Athlete's foot, also known as tinea pedis, can be an extremely contagious foot infection. It is commonly contracted in public changing areas and bathrooms, dormitory style living quarters, around locker rooms and public swimming pools, or anywhere your feet often come into contact with other people.
Solutions to Combat Athlete’s Foot
- Hydrate your feet by using lotion
- Exfoliate
- Buff off nails
- Use of anti-fungal products
- Examine your feet and visit your doctor if any suspicious blisters or cuts develop
Athlete’s foot can cause many irritating symptoms such as dry and flaking skin, itching, and redness. Some more severe symptoms can include bleeding and cracked skin, intense itching and burning, and even pain when walking. In the worst cases, Athlete’s foot can cause blistering as well. Speak to your podiatrist for a better understanding of the different causes of Athlete’s foot, as well as help in determining which treatment options are best for you.
If you have any questions please feel free to contact one of our offices located in Bellevue, Seattle, and Issaquah, WA, . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Why Diabetics Are Prone to Developing Foot Ulcers
Foot ulcers are open wounds that may be clearly visible or hidden beneath hardened skin or dead tissue. They can occur on the bottom or sides of the foot, or on the top or tip of the toes, and range in severity from surface wounds to deep craters that may expose tendons and bones. Left undetected and untreated, they may become infected and escalate to a serious health issue. In the worst cases, foot ulcers may even lead to amputation. Discovering and healing ulcers can be challenging for those with diabetes. Increased levels of glucose in the blood may cause nerve damage and poor circulation, which may decrease your ability to detect and heal ulcers. Along with treating other foot and ankle issues, podiatrists can provide proper diabetic foot ulcer care through a variety of treatments, medicines, and procedures.
Wound care is an important part in dealing with diabetes. If you have diabetes and a foot wound or would like more information about wound care for diabetics, consult with one of our podiatrists from Grobowski Foot & Ankle. our doctors will assess your condition and provide you with quality foot and ankle treatment.
What Is Wound Care?
Wound care is the practice of taking proper care of a wound. This can range from the smallest to the largest of wounds. While everyone can benefit from proper wound care, it is much more important for diabetics. Diabetics often suffer from poor blood circulation which causes wounds to heal much slower than they would in a non-diabetic.
What Is the Importance of Wound Care?
While it may not seem apparent with small ulcers on the foot, for diabetics, any size ulcer can become infected. Diabetics often also suffer from neuropathy, or nerve loss. This means they might not even feel when they have an ulcer on their foot. If the wound becomes severely infected, amputation may be necessary. Therefore, it is of the upmost importance to properly care for any and all foot wounds.
How to Care for Wounds
The best way to care for foot wounds is to prevent them. For diabetics, this means daily inspections of the feet for any signs of abnormalities or ulcers. It is also recommended to see a podiatrist several times a year for a foot inspection. If you do have an ulcer, run the wound under water to clear dirt from the wound; then apply antibiotic ointment to the wound and cover with a bandage. Bandages should be changed daily and keeping pressure off the wound is smart. It is advised to see a podiatrist, who can keep an eye on it.
If you have any questions, please feel free to contact one of our offices located in Bellevue, Seattle, and Issaquah, WA, . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Wounds That Don't Heal Need to Be Checked
Two Tiny Bones and a Big Toe
Sesamoids are tiny bones located within tendons that connect to muscles—as opposed to most bones which link to one another via joints. The patella, or kneecap, is the largest sesamoid, while the two sesamoids on the bottom of the feet near the big toe (the tibial and the fibular) are pea-sized. Despite their small size, these two sesamoids bear the body’s weight and the tendons they are attached to can become inflamed if they are overly stressed from high heels or activities such as ballet, basketball, or running. This condition is called sesamoiditis and can cause gradually-worsening pain under the ball of the foot, and popping sensations or difficulty bending the big toe. If you experience any of these symptoms, a podiatrist can thoroughly examine you and may utilize an X-ray, bone scan, MRI or ultrasound to determine if you have sesamoiditis. Treatment may involve lifestyle or footwear modifications, medications, or orthotics. Severe cases of sesamoiditis that do not respond to traditional treatment may require surgery.
Sesamoiditis is an unpleasant foot condition characterized by pain in the balls of the feet. If you think you’re struggling with sesamoiditis, contact one of our podiatrists of Grobowski Foot & Ankle. our doctors will treat your condition thoroughly and effectively.
Sesamoiditis
Sesamoiditis is a condition of the foot that affects the ball of the foot. It is more common in younger people than it is in older people. It can also occur with people who have begun a new exercise program, since their bodies are adjusting to the new physical regimen. Pain may also be caused by the inflammation of tendons surrounding the bones. It is important to seek treatment in its early stages because if you ignore the pain, this condition can lead to more serious problems such as severe irritation and bone fractures.
Causes of Sesamoiditis
- Sudden increase in activity
- Increase in physically strenuous movement without a proper warm up or build up
- Foot structure: those who have smaller, bonier feet or those with a high arch may be more susceptible
Treatment for sesamoiditis is non-invasive and simple. Doctors may recommend a strict rest period where the patient forgoes most physical activity. This will help give the patient time to heal their feet through limited activity. For serious cases, it is best to speak with your doctor to determine a treatment option that will help your specific needs.
If you have any questions please feel free to contact one of our offices located in Bellevue, Seattle, and Issaquah, WA, . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Are Tarsal Tunnel Syndrome and Carpal Tunnel Similar?
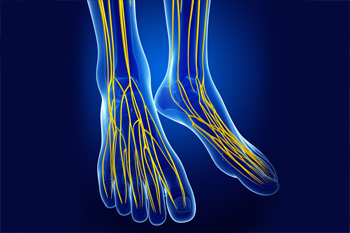
The tarsal tunnel is a narrow passageway on the inside of the ankle that protects the veins, tendons, arteries and nerves within it, such as the tibial nerve. Tarsal tunnel syndrome occurs when the tibial nerve becomes compressed. Symptoms range from a shooting pain, numbness, or a burning/tingling sensation anywhere along the tibial nerve from the ankle down through the heel, arch, and even toes. Tarsal tunnel syndrome is similar to carpal tunnel syndrome (which occurs in the wrist) in that both conditions involve a nerve being compressed within a confined space. Common causes of tarsal tunnel syndrome include flat feet, ankle sprains, diabetes and arthritis, and other conditions that contribute to compressing, or squeezing the tibial nerve. It’s important to seek prompt treatment for tarsal tunnel syndrome because if left untreated the condition may permanently damage the tibial nerve. If you believe you are suffering from tarsal tunnel syndrome, contact a podiatrist who can properly diagnose your condition and provide a variety of treatments and therapies.
Tarsal tunnel syndrome can be very uncomfortable to live with. If you are experiencing tarsal tunnel syndrome, contact one of our podiatrists of Grobowski Foot & Ankle. our doctors can provide the care you need to keep you pain-free and on your feet.
Tarsal Tunnel Syndrome
Tarsal tunnel syndrome, which can also be called tibial nerve dysfunction, is an uncommon condition of misfiring peripheral nerves in the foot. The tibial nerve is the peripheral nerve in the leg responsible for sensation and movement of the foot and calf muscles. In tarsal tunnel syndrome, the tibial nerve is damaged, causing problems with movement and feeling in the foot of the affected leg.
Common Cause of Tarsal Tunnel Syndrome
- Involves pressure or an injury, direct pressure on the tibial nerve for an extended period of time, sometimes caused by other body structures close by or near the knee.
- Diseases that damage nerves, including diabetes, may cause tarsal tunnel syndrome.
- At times, tarsal tunnel syndrome can appear without an obvious cause in some cases.
The Effects of Tarsal Tunnel Syndrome
- Different sensations, an afflicted person may experience pain, tingling, burning or other unusual sensations in the foot of the affected leg.
- The foot muscles, toes and ankle become weaker, and curling your toes or flexing your foot can become difficult.
- If condition worsens, infections and ulcers may develop on the foot that is experiencing the syndrome.
A physical exam of the leg can help identify the presence of tarsal tunnel syndrome. Medical tests, such as a nerve biopsy, are also used to diagnose the condition. Patients may receive physical therapy and prescriptive medication. In extreme cases, some may require surgery.
If you have any questions please feel free to contact one of our offices located in Bellevue, Seattle, and Issaquah, WA, . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.