Connect With Us
Blog

Toenail fungus often starts as a small change in color or texture. The nail may look yellow, white or brown, and become thick, brittle, or crumbly over time. It can spread to other nails and may cause odor or discomfort. Fungal infections thrive in warm, moist places such as sweaty shoes or public showers. Early treatment can stop it from getting worse. Creams may help in mild cases, but deeper infections often need prescription medication. Keeping nails trimmed, dry, and clean helps prevent infection. Avoid walking barefoot in shared spaces and change socks often. Toenail fungus rarely goes away on its own. If your nail is changing in appearance or causing discomfort, it is suggested you see a podiatrist for professional treatment.
If left untreated, toenail fungus may spread to other toenails, skin, or even fingernails. If you suspect you have toenail fungus it is important to seek treatment right away. For more information about treatment, contact one of our podiatrists of Grobowski Foot & Ankle. our doctors can provide the care you need to keep you pain-free and on your feet.
Symptoms
- Warped or oddly shaped nails
- Yellowish nails
- Loose/separated nail
- Buildup of bits and pieces of nail fragments under the nail
- Brittle, broken, thickened nail
Treatment
If self-care strategies and over-the-counter medications does not help your fungus, your podiatrist may give you a prescription drug instead. Even if you find relief from your toenail fungus symptoms, you may experience a repeat infection in the future.
Prevention
In order to prevent getting toenail fungus in the future, you should always make sure to wash your feet with soap and water. After washing, it is important to dry your feet thoroughly especially in between the toes. When trimming your toenails, be sure to trim straight across instead of in a rounded shape. It is crucial not to cover up discolored nails with nail polish because that will prevent your nail from being able to “breathe”.
In some cases, surgical procedure may be needed to remove the toenail fungus. Consult with your podiatrist about the best treatment options for your case of toenail fungus.
If you have any questions, please feel free to contact one of our offices located in Bellevue, Seattle, and Issaquah, WA, . We offer the newest diagnostic and treatment technologies for all your foot care needs.

The feet can often reveal early signs of liver problems that might otherwise go unnoticed. One common indication is the appearance of spider veins, which are small, visible blood vessels that can form on the feet and ankles when the liver is not properly filtering blood. Cracked heels may also suggest liver dysfunction, as poor circulation and dehydration associated with liver issues can lead to dry, splitting skin. Another sign to watch for is white nail beds, which can signal a lack of healthy blood flow or low protein levels caused by liver disease. These changes in the feet may seem minor at first, but they can provide important clues about underlying liver health. If you notice any changes to your feet, it is suggested that you consult a podiatrist who can treat various foot conditions, and guide you if an underlying health issue is a concern.
When dealing with systemic disease of the feet, it is extremely important to check the affected areas routinely so that any additional problems are caught quickly. If you have any concerns about your feet and ankles contact one of our podiatrists from Grobowski Foot & Ankle. our doctors will assist you with all of your podiatric needs.
Systemic Diseases of the Feet
Systemic diseases affect the whole body, and symptoms usually are displayed in the feet. This condition can make a patient’s ability to walk unbearable. Systemic diseases include gout, diabetes mellitus, neurological disorders, and arthritis.
Gout – is caused by an excess of uric acid in the body. Common symptoms include pain, inflammation, and redness at the metatarsal/phalangeal joint of the base big toe. Gout can be treated by NSAIDs to relieve pain and inflammation, and other drugs that lower the acid levels in the body.
Diabetes mellitus – is an increase in the level of blood sugar that the body cannot counteract with its own insulin. Failure to produce enough insulin is a factor in Diabetes.
Diabetes of the Feet
Diabetic Neuropathy – may lead to damaged nerves and affect the feet through numbness and loss of sensation.
Peripheral Vascular Disease – can restrict the blood flow to the feet, and often times lead to amputation of the feet.
If you have any questions please feel free to contact one of our offices located in Bellevue, Seattle, and Issaquah, WA, . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
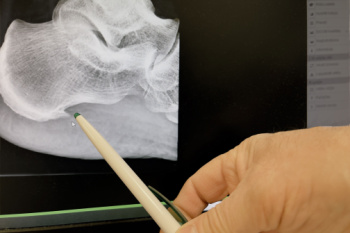
A heel spur is a bony growth that forms on the underside of the heel bone, often linked with long-term strain on foot muscles and ligaments. It develops when calcium deposits build up over time, creating a pointed projection that can cause heel pain, especially during walking or standing. Heel spurs are commonly associated with plantar fasciitis, a condition involving inflammation of the connective tissue along the bottom of the foot. Diagnosis is typically confirmed through physical examination and imaging studies like X-rays. Contributing causes include repetitive stress from activities like running, wearing unsupportive footwear, or having flat feet or high arches. Risk factors include aging, obesity, and occupations that involve prolonged standing. If you have heel pain, it is suggested that you schedule an appointment with a podiatrist who can accurately diagnose and treat heel spurs.
Heel spurs can be incredibly painful and sometimes may make you unable to participate in physical activities. To get medical care for your heel spurs, contact one of our podiatrists from Grobowski Foot & Ankle. our doctors will do everything possible to treat your condition.
Heels Spurs
Heel spurs are formed by calcium deposits on the back of the foot where the heel is. This can also be caused by small fragments of bone breaking off one section of the foot, attaching onto the back of the foot. Heel spurs can also be bone growth on the back of the foot and may grow in the direction of the arch of the foot.
Older individuals usually suffer from heel spurs and pain sometimes intensifies with age. One of the main condition's spurs are related to is plantar fasciitis.
Pain
The pain associated with spurs is often because of weight placed on the feet. When someone is walking, their entire weight is concentrated on the feet. Bone spurs then have the tendency to affect other bones and tissues around the foot. As the pain continues, the feet will become tender and sensitive over time.
Treatments
There are many ways to treat heel spurs. If one is suffering from heel spurs in conjunction with pain, there are several methods for healing. Medication, surgery, and herbal care are some options.
If you have any questions feel free to contact one of our offices located in Bellevue, Seattle, and Issaquah, WA, . We offer the latest in diagnostic and treatment technology to meet your needs.
Featured Articles
- May 2025
- April 2025
- March 2025
- February 2025
- January 2025
- December 2024
- November 2024
- October 2024
- September 2024
- August 2024
- July 2024
- June 2024
- May 2024
- April 2024
- March 2024
- February 2024
- January 2024
- December 2023
- November 2023
- October 2023
- September 2023
- August 2023
- July 2023
- June 2023
- May 2023
- April 2023
- March 2023
- February 2023
- January 2023
- December 2022
- November 2022
- October 2022
- September 2022
- August 2022
- July 2022
- June 2022
- May 2022
- April 2022
- March 2022
- February 2022
- January 2022
- December 2021
- November 2021
- October 2021
- September 2021
- August 2021
- July 2021
- June 2021
- May 2021
- April 2021
- March 2021
- February 2021
- January 2021
- December 2020
- November 2020
- October 2020
- September 2020
- August 2020
- July 2020
- June 2020
- May 2020
- April 2020
- March 2020
- February 2020
- January 2020
- December 2019
- November 2019
- October 2019
- September 2019
- August 2019
- July 2019
- June 2019
- May 2019
- April 2019
- March 2019
- February 2019
- January 2019
- December 2018
- November 2018
- October 2018
- September 2018
- August 2018