Connect With Us
Featured Articles
Super User
Possible Causes of Plantar Fasciitis
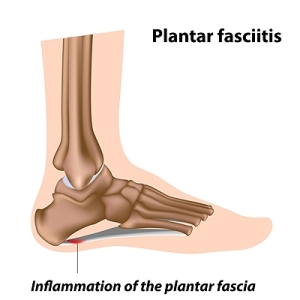
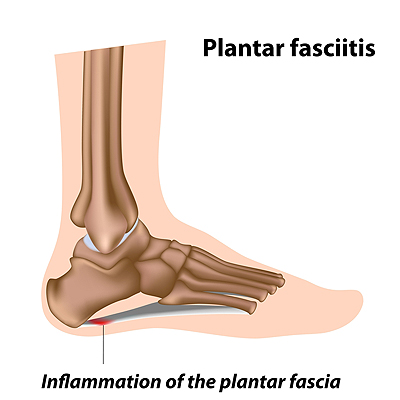 There is a portion of tissue that is located on the bottom of the foot that is known as the plantar fascia. It connects the heel to the toes, and a healthy plantar fascia is crucial in performing daily functions. There are certain activities that can cause the condition that is referred to as plantar fasciitis, and this can cause severe pain and discomfort. Plantar fasciitis can gradually develop as a result of standing on hard surfaces for the majority of the day, or it may come from wearing shoes that do not fit correctly. Many people who enjoy running may experience this type of foot condition, and it may happen from consistent pressure that is put on the heels. If you have developed plantar fasciitis, it is suggested that you seek the counsel of a podiatrist who can properly treat this condition.
There is a portion of tissue that is located on the bottom of the foot that is known as the plantar fascia. It connects the heel to the toes, and a healthy plantar fascia is crucial in performing daily functions. There are certain activities that can cause the condition that is referred to as plantar fasciitis, and this can cause severe pain and discomfort. Plantar fasciitis can gradually develop as a result of standing on hard surfaces for the majority of the day, or it may come from wearing shoes that do not fit correctly. Many people who enjoy running may experience this type of foot condition, and it may happen from consistent pressure that is put on the heels. If you have developed plantar fasciitis, it is suggested that you seek the counsel of a podiatrist who can properly treat this condition.
Plantar fasciitis can be very painful and inconvenient. If you are experiencing heel pain or symptoms of plantar fasciitis, contact one of our podiatrists from Grobowski Foot & Ankle. our doctors can provide the care you need to keep you pain-free and on your feet.
What Is Plantar Fasciitis?
Plantar fasciitis is the inflammation of the thick band of tissue that runs along the bottom of your foot, known as the plantar fascia, and causes mild to severe heel pain.
What Causes Plantar Fasciitis?
- Excessive running
- Non-supportive shoes
- Overpronation
- Repeated stretching and tearing of the plantar fascia
How Can It Be Treated?
- Conservative measures – anti-inflammatories, ice packs, stretching exercises, physical therapy, orthotic devices
- Shockwave therapy – sound waves are sent to the affected area to facilitate healing and are usually used for chronic cases of plantar fasciitis
- Surgery – usually only used as a last resort when all else fails. The plantar fascia can be surgically detached from the heel
While very treatable, plantar fasciitis is definitely not something that should be ignored. Especially in severe cases, speaking to your doctor right away is highly recommended to avoid complications and severe heel pain. Your podiatrist can work with you to provide the appropriate treatment options tailored to your condition.
If you have any questions please feel free to contact one of our offices located in Bellevue, Seattle, and Issaquah, WA, . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Where Do Plantar Warts Develop?
A growth on the sole of the foot may indicate a plantar wart. A plantar wart is described as a small, thick patch of skin that grows into the bottom of the foot. This happens as a result of the constant pressure the feet endure by walking, standing, and running. This type of wart is caused by a virus that is known as the human papillomavirus (HPV), and is considered to be contagious. Common symptoms that are often seen with plantar warts can include severe pain and discomfort while walking, and the wart may have small black dots in the center, which is dried blood. There are a variety of methods to treat plantar warts, consisting of applying salicylic acid directly on the wart, utilizing cryotherapy, or other forms of medicine. If you have developed this type of wart, it is suggested that you consult with a podiatrist who can effectively treat plantar warts.
Plantar warts can be very uncomfortable. If you need your feet checked, contact one of our podiatrists from Grobowski Foot & Ankle. our doctors will assist you with all of your foot and ankle needs.
About Plantar Warts
Plantar warts are the result of HPV, or human papillomavirus, getting into open wounds on the feet. They are mostly found on the heels or balls of the feet.
While plantar warts are generally harmless, those experiencing excessive pain or those suffering from diabetes or a compromised immune system require immediate medical care. Plantar warts are easily diagnosed, usually through scraping off a bit of rough skin or by getting a biopsy.
Symptoms
- Lesions on the bottom of your feet, usually rough and grainy
- Hard or thick callused spots
- Wart seeds, which are small clotted blood vessels that look like little black spots
- Pain, discomfort, or tenderness of your feet when walking or standing
Treatment
- Freezing
- Electric tool removal
- Laser Treatment
- Topical Creams (prescription only)
- Over-the-counter medications
To help prevent developing plantar warts, avoid walking barefoot over abrasive surfaces that can cause cuts or wounds for HPV to get into. Avoiding direct contact with other warts, as well as not picking or rubbing existing warts, can help prevent the further spread of plantar warts. However, if you think you have developed plantar warts, speak to your podiatrist. He or she can diagnose the warts on your feet and recommend the appropriate treatment options.
If you have any questions please feel free to contact one of our offices located in Bellevue, Seattle, and Issaquah, WA, . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Where Is the Achilles Tendon Located?
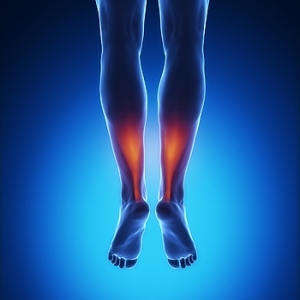
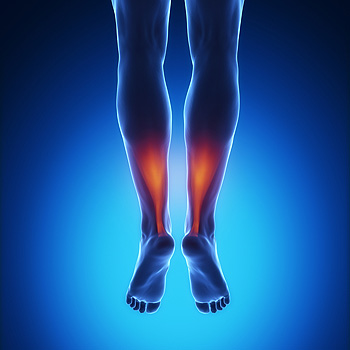 The medical term for the Achilles tendon is the calcaneal tendon. It is located in the back of the leg, and connects the calf muscles to the heel. It is considered to be one of the longest tendons in the body, and is used during walking and running activities. An injury to the Achilles tendon may occur as a result of not warming up adequately before beginning an exercise program. Achilles tendonitis or a rupture can cause severe pain and discomfort. Patients may be susceptible to experiencing this type of injury with existing flat feet or tight calf muscles. There are prevention techniques that can be implemented which may help to reduce the risk of incurring an Achilles tendon injury. These can include stretching before any type of exercise is pursued, in addition to wearing shoes that fit correctly. If you have pain in your heel or if your calf muscles are stiff, please consult with a podiatrist who can properly diagnose and treat Achilles tendon injuries.
The medical term for the Achilles tendon is the calcaneal tendon. It is located in the back of the leg, and connects the calf muscles to the heel. It is considered to be one of the longest tendons in the body, and is used during walking and running activities. An injury to the Achilles tendon may occur as a result of not warming up adequately before beginning an exercise program. Achilles tendonitis or a rupture can cause severe pain and discomfort. Patients may be susceptible to experiencing this type of injury with existing flat feet or tight calf muscles. There are prevention techniques that can be implemented which may help to reduce the risk of incurring an Achilles tendon injury. These can include stretching before any type of exercise is pursued, in addition to wearing shoes that fit correctly. If you have pain in your heel or if your calf muscles are stiff, please consult with a podiatrist who can properly diagnose and treat Achilles tendon injuries.
Achilles tendon injuries need immediate attention to avoid future complications. If you have any concerns, contact one of our podiatrists of Grobowski Foot & Ankle. our doctors can provide the care you need to keep you pain-free and on your feet.
What Is the Achilles Tendon?
The Achilles tendon is a tendon that connects the lower leg muscles and calf to the heel of the foot. It is the strongest tendon in the human body and is essential for making movement possible. Because this tendon is such an integral part of the body, any injuries to it can create immense difficulties and should immediately be presented to a doctor.
What Are the Symptoms of an Achilles Tendon Injury?
There are various types of injuries that can affect the Achilles tendon. The two most common injuries are Achilles tendinitis and ruptures of the tendon.
Achilles Tendinitis Symptoms
- Inflammation
- Dull to severe pain
- Increased blood flow to the tendon
- Thickening of the tendon
Rupture Symptoms
- Extreme pain and swelling in the foot
- Total immobility
Treatment and Prevention
Achilles tendon injuries are diagnosed by a thorough physical evaluation, which can include an MRI. Treatment involves rest, physical therapy, and in some cases, surgery. However, various preventative measures can be taken to avoid these injuries, such as:
- Thorough stretching of the tendon before and after exercise
- Strengthening exercises like calf raises, squats, leg curls, leg extensions, leg raises, lunges, and leg presses
If you have any questions please feel free to contact one of our offices located in Bellevue, Seattle, and Issaquah, WA, . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.
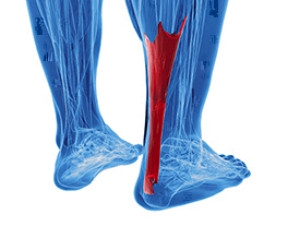
What are Achilles Tendon Injuries
The Achilles tendon is the strongest tendon in the human body. Its purpose is to connect the lower leg muscles and calf to the heel of the foot. This tendon is responsible for facilitating all types of movement, like walking and running. This tendon provides an enormous amount of mobility for the body. Any injuries inflicted to this tissue should be immediately brought up with a physician to prevent further damage.
The most common injuries that can trouble the Achilles tendon are tendon ruptures and Achilles tendinitis. Achilles tendinitis is the milder of the two injuries. It can be recognized by the following symptoms: inflammation, dull-to-severe pain, increased blood flow to the tendon, thickening of the tendon, and slower movement time. Tendinitis can be treated via several methods and is often diagnosed by an MRI.
An Achilles tendon rupture is trickier to heal, and is by far the most painful injury. It is caused by the tendon ripping or completely snapping. The results are immediate and absolutely devastating, and will render the patient immobile. If a rupture or tear occurs, operative and non-operative methods are available. Once the treatment begins, depending on the severity of the injury, recovery time for these types of issues can take up to a year.
Simple preventative measures can be taken as a means to avoid both injuries. Prior to any movement, taking a few minutes to stretch out the tendon is a great way to stimulate the tissue. Calf raises, squats, leg curls, leg extensions, leg raises, lunges, and leg presses are all suggested ways to help strengthen the lower legs and promote Achilles tendon health.
Many problems arise among athletes and people who overexert themselves while exercising. Problems can also happen among those who do not warm up properly before beginning an activity. Proper, comfortable shoes that fit correctly can also decrease tendon injuries. Some professionals also suggest that when exercising, you should make sure that the floor you are on is cushioned or has a mat. This will relieve pressure on the heels. A healthy diet will also increase tendon health.
It is very important to seek out a podiatrist if you believe you have an injury in the Achilles region. Further damage could result in severe complications that would make being mobile difficult, if not impossible.
Defining an Achilles Tendon Rupture
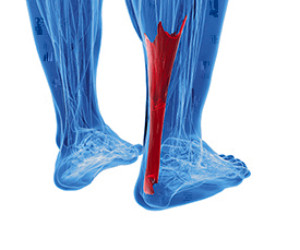 The Achilles tendon, located at the back of the ankle, connects the calf muscle to the heel bone. When the tendon gets overstretched because of forceful jumping, pivoting, or sudden acceleration, the tendon can tear or rupture. Some signs of an Achilles tendon tear includes sudden pain in the calf or ankle, swelling in the back of the leg, a popping sensation, and difficulty walking. An Achilles tendon rupture is a very serious injury that will require the care of a podiatrist to prevent further damage. Treatments that a podiatrist may recommend can include a walking boot, or in severe cases, surgery. Physical therapy will likely be necessary to aid in the recovery process as well. If you are afflicted with an Achilles tendon injury, please consult with a podiatrist for the best treatment techniques that are correct for you.
The Achilles tendon, located at the back of the ankle, connects the calf muscle to the heel bone. When the tendon gets overstretched because of forceful jumping, pivoting, or sudden acceleration, the tendon can tear or rupture. Some signs of an Achilles tendon tear includes sudden pain in the calf or ankle, swelling in the back of the leg, a popping sensation, and difficulty walking. An Achilles tendon rupture is a very serious injury that will require the care of a podiatrist to prevent further damage. Treatments that a podiatrist may recommend can include a walking boot, or in severe cases, surgery. Physical therapy will likely be necessary to aid in the recovery process as well. If you are afflicted with an Achilles tendon injury, please consult with a podiatrist for the best treatment techniques that are correct for you.
Achilles tendon injuries need immediate attention to avoid future complications. If you have any concerns, contact one of our podiatrists of Grobowski Foot & Ankle. our doctors can provide the care you need to keep you pain-free and on your feet.
What Is the Achilles Tendon?
The Achilles tendon is a tendon that connects the lower leg muscles and calf to the heel of the foot. It is the strongest tendon in the human body and is essential for making movement possible. Because this tendon is such an integral part of the body, any injuries to it can create immense difficulties and should immediately be presented to a doctor.
What Are the Symptoms of an Achilles Tendon Injury?
There are various types of injuries that can affect the Achilles tendon. The two most common injuries are Achilles tendinitis and ruptures of the tendon.
Achilles Tendinitis Symptoms
- Inflammation
- Dull to severe pain
- Increased blood flow to the tendon
- Thickening of the tendon
Rupture Symptoms
- Extreme pain and swelling in the foot
- Total immobility
Treatment and Prevention
Achilles tendon injuries are diagnosed by a thorough physical evaluation, which can include an MRI. Treatment involves rest, physical therapy, and in some cases, surgery. However, various preventative measures can be taken to avoid these injuries, such as:
- Thorough stretching of the tendon before and after exercise
- Strengthening exercises like calf raises, squats, leg curls, leg extensions, leg raises, lunges, and leg presses
If you have any questions please feel free to contact one of our offices located in Bellevue, Seattle, and Issaquah, WA, . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.
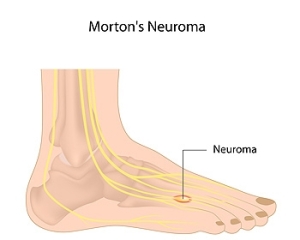
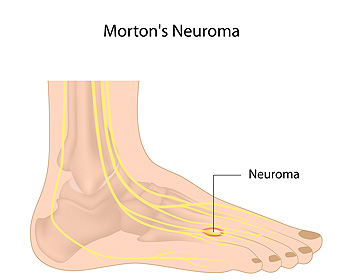
Location of Pain Caused by Morton’s Neuroma
A nerve tissue that has become thickened is referred to as a neuroma. If the tissue that is found between the toes near the ball of the foot becomes inflamed, it is a condition that is known as Morton’s neuroma. It can happen as a result of wearing shoes that are too narrow, or from participating in sporting activities where pressure is placed on the front of the foot. Additionally, it may develop from existing foot deformities that can include flat feet and bunions. A noticeable symptom that patients could have is a burning pain on the sole of the foot, which may travel to the toes. Mild relief may be found when orthotics are worn, and this may give the affected foot the support that is needed as the pressure is reduced. It can be beneficial to avoid wearing high heels, and choosing to wear shoes that are wider in the toe area may be more comfortable. If you have a sharp pain on the bottom of your foot, it is suggested that you speak with a podiatrist who can properly diagnose and treat Morton’s neuroma.
Morton’s neuroma is a very uncomfortable condition to live with. If you think you have Morton’s neuroma, contact one of our podiatrists of Grobowski Foot & Ankle. our doctors will attend to all of your foot care needs and answer any of your related questions.
Morton’s Neuroma
Morton's neuroma is a painful foot condition that commonly affects the areas between the second and third or third and fourth toe, although other areas of the foot are also susceptible. Morton’s neuroma is caused by an inflamed nerve in the foot that is being squeezed and aggravated by surrounding bones.
What Increases the Chances of Having Morton’s Neuroma?
- Ill-fitting high heels or shoes that add pressure to the toe or foot
- Jogging, running or any sport that involves constant impact to the foot
- Flat feet, bunions, and any other foot deformities
Morton’s neuroma is a very treatable condition. Orthotics and shoe inserts can often be used to alleviate the pain on the forefront of the feet. In more severe cases, corticosteroids can also be prescribed. In order to figure out the best treatment for your neuroma, it’s recommended to seek the care of a podiatrist who can diagnose your condition and provide different treatment options.
If you have any questions, please feel free to contact one of our offices located in Bellevue, Seattle, and Issaquah, WA, . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Morton's Neuroma
A neuroma is a thickening of nerve tissue and can develop throughout the body. In the foot, the most common neuroma is a Morton’s neuroma; this typically forms between the third and fourth toes. The thickening of the nerve is typically caused by compression and irritation of the nerve; this thickening can in turn cause enlargement and, in some cases, nerve damage.
Neuromas can be caused by anything that causes compression or irritation of the nerve. A common cause is wearing shoes with tapered toe boxes or high heels that force the toes into the toe boxes. Physical activities that involve repeated pressure to the foot, such as running or basketball, can also create neuromas. Those with foot deformities, such as bunions, hammertoes, or flatfeet, are more likely to develop the condition.
Symptoms of Morton’s neuroma include tingling, burning, numbness, pain, and the feeling that either something is inside the ball of the foot or that something in one’s shoe or sock is bunched up. Symptoms typically begin gradually and can even go away temporarily by removing one’s shoes or massaging the foot. An increase in the intensity of symptoms correlates with the increasing growth of the neuroma.
Treatment for Morton’s neuroma can vary between patients and the severity of the condition. For mild to moderate cases, padding, icing, orthotics, activity modifications, shoe modifications, medications, and injection therapy may be suggested or prescribed. Patients who have not responded successfully to less invasive treatments may require surgery to properly treat their condition. The severity of your condition will determine the procedure performed and the length of recovery afterwards.
Treating a Blister
 Blisters often form on the feet as a defense against damage to the skin. They take the form of fluid filled sacs on the outer layer of the skin of the feet, often developing in response to excess friction. Most commonly, blisters form because of ill-fitting footwear rubbing against the skin. Blisters themselves are wounds that will slowly heal on their own, however they can cause a great deal of discomfort. Other reasons why blisters may form can include sunburns, frostbite, eczema, allergic reactions, viral infections, and bacterial infections. To help heal a blister, it’s best to leave it alone. As stated before, they will heal on their own. It may be beneficial to protect the blister by covering it up with a bandage. Some natural remedies to help heal a blister can include applying aloe vera, as well as green tea, tea tree oil, and eucalyptus oil. For more information on how to help treat a blister, it’s suggested that you speak with a podiatrist.
Blisters often form on the feet as a defense against damage to the skin. They take the form of fluid filled sacs on the outer layer of the skin of the feet, often developing in response to excess friction. Most commonly, blisters form because of ill-fitting footwear rubbing against the skin. Blisters themselves are wounds that will slowly heal on their own, however they can cause a great deal of discomfort. Other reasons why blisters may form can include sunburns, frostbite, eczema, allergic reactions, viral infections, and bacterial infections. To help heal a blister, it’s best to leave it alone. As stated before, they will heal on their own. It may be beneficial to protect the blister by covering it up with a bandage. Some natural remedies to help heal a blister can include applying aloe vera, as well as green tea, tea tree oil, and eucalyptus oil. For more information on how to help treat a blister, it’s suggested that you speak with a podiatrist.
Blisters may appear as a single bubble or in a cluster. They can cause a lot of pain and may be filled with pus, blood, or watery serum. If your feet are hurting, contact one of our podiatrists of Grobowski Foot & Ankle. our doctors can provide the care you need to keep you pain-free and on your feet.
Foot Blisters
Foot blisters are often the result of friction. This happens due to the constant rubbing from shoes, which can lead to pain.
What Are Foot Blisters?
A foot blister is a small fluid-filled pocket that forms on the upper-most layer of the skin. Blisters are filled with clear fluid and can lead to blood drainage or pus if the area becomes infected.
Symptoms
(Blister symptoms may vary depending on what is causing them)
- Bubble of skin filled with fluid
- Redness
- Moderate to severe pain
- Itching
Prevention & Treatment
In order to prevent blisters, you should be sure to wear comfortable shoes with socks that cushion your feet and absorb sweat. Breaking a blister open may increase your chances of developing an infection. However, if your blister breaks, you should wash the area with soap and water immediately and then apply a bandage to the affected area. If your blisters cause severe pain it is important that you call your podiatrist right away.
If you have any questions, please feel free to contact one of our offices located in Bellevue, Seattle, and Issaquah, WA, . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Read more about Blisters on the FeetHeel Spur Symptoms
 Patients who experience heel pain may be aware that this can be indicative of a heel spur. This is defined as a small piece of bone that grows on the inside of the heel and is often confused with plantar fasciitis. It can develop from a strained plantar fascia, which may be a result of wearing shoes that do not fit correctly. Common symptoms that often accompany heel spurs include pain and discomfort in the heel and surrounding areas, and it is often difficult to perform daily activities. Patients may find comfort in practicing specific foot stretches that can help to relax the tissues near the heel, and relief may be found when the affected foot is rested and elevated. It is strongly advised that you consult with a podiatrist who can determine the cause of existing heel pain, and offer correct treatment options for heel spurs.
Patients who experience heel pain may be aware that this can be indicative of a heel spur. This is defined as a small piece of bone that grows on the inside of the heel and is often confused with plantar fasciitis. It can develop from a strained plantar fascia, which may be a result of wearing shoes that do not fit correctly. Common symptoms that often accompany heel spurs include pain and discomfort in the heel and surrounding areas, and it is often difficult to perform daily activities. Patients may find comfort in practicing specific foot stretches that can help to relax the tissues near the heel, and relief may be found when the affected foot is rested and elevated. It is strongly advised that you consult with a podiatrist who can determine the cause of existing heel pain, and offer correct treatment options for heel spurs.
Heel spurs can be incredibly painful and sometimes may make you unable to participate in physical activities. To get medical care for your heel spurs, contact one of our podiatrists from Grobowski Foot & Ankle. our doctors will do everything possible to treat your condition.
Heels Spurs
Heel spurs are formed by calcium deposits on the back of the foot where the heel is. This can also be caused by small fragments of bone breaking off one section of the foot, attaching onto the back of the foot. Heel spurs can also be bone growth on the back of the foot and may grow in the direction of the arch of the foot.
Older individuals usually suffer from heel spurs and pain sometimes intensifies with age. One of the main condition's spurs are related to is plantar fasciitis.
Pain
The pain associated with spurs is often because of weight placed on the feet. When someone is walking, their entire weight is concentrated on the feet. Bone spurs then have the tendency to affect other bones and tissues around the foot. As the pain continues, the feet will become tender and sensitive over time.
Treatments
There are many ways to treat heel spurs. If one is suffering from heel spurs in conjunction with pain, there are several methods for healing. Medication, surgery, and herbal care are some options.
If you have any questions feel free to contact one of our offices located in Bellevue, Seattle, and Issaquah, WA, . We offer the latest in diagnostic and treatment technology to meet your needs.
How to Treat Heel Spurs
Heel spurs are calcium deposits that cause bone protrusions on the heel bone. Heel spurs are usually associated with plantar fasciitis, which occurs when the plantar fasciitis in the foot becomes inflamed. Typically, heel spurs don’t cause any symptoms. However, they can produce chronic or intermittent heel pain. Those who have had the condition often describe the irritation as a stabbing pain.
There are risk factors that may make you more likely to develop heel spurs. People who have abnormal walking gaits, run and jog on hard surfaces, are obese, or wear poorly fitting shoes are more likely to develop heel spurs.
Fortunately, there are precautions you can take to avoid developing heel spurs. One of the best ways to do this is by wearing well-fitting shoes with shock-absorbent soles. Another preventative technique is to choose running shoes if you plan on running, and walking shoes if you plan on walking. Shoes are made for different activities and it is important to research a shoe before you purchase a pair.
The pain associated with heel spurs often decreases the more you walk. However, a recurrence of pain after an extended period of rest or walking is likely to occur with this condition. Those with severe heel spur pain may opt to go the surgical route for treatment. However, more than 90% of those with the condition get better without surgical treatment. If you have a heel spur and want to know if surgery is right for you, you should go to your podiatrist and he or she will be able to conduct a pre-surgical test or exam to determine if you are an optimal candidate for surgery.
Featured Articles
- April 2025
- March 2025
- February 2025
- January 2025
- December 2024
- November 2024
- October 2024
- September 2024
- August 2024
- July 2024
- June 2024
- May 2024
- April 2024
- March 2024
- February 2024
- January 2024
- December 2023
- November 2023
- October 2023
- September 2023
- August 2023
- July 2023
- June 2023
- May 2023
- April 2023
- March 2023
- February 2023
- January 2023
- December 2022
- November 2022
- October 2022
- September 2022
- August 2022
- July 2022
- June 2022
- May 2022
- April 2022
- March 2022
- February 2022
- January 2022
- December 2021
- November 2021
- October 2021
- September 2021
- August 2021
- July 2021
- June 2021
- May 2021
- April 2021
- March 2021
- February 2021
- January 2021
- December 2020
- November 2020
- October 2020
- September 2020
- August 2020
- July 2020
- June 2020
- May 2020
- April 2020
- March 2020
- February 2020
- January 2020
- December 2019
- November 2019
- October 2019
- September 2019
- August 2019
- July 2019
- June 2019
- May 2019
- April 2019
- March 2019
- February 2019
- January 2019
- December 2018
- November 2018
- October 2018
- September 2018
- August 2018